We treat the Person, not the Picture
As a chiropractic clinic, we are often asked why we don’t take x-rays on the first visit. Our answer is an x-ray is a good diagnostic imaging tool in the right scenario. However, in chiropractic clinics and other medical facilities, x-rays, and other imaging studies, like MRIs, are overutilized and can create a big problem. This article is meant to clear up any confusion when it comes to x-ray imaging and give an insight into when it’s most appropriate to order advanced images (CT scan, MRI, etc.).
When should x-rays or MRIs be used?
-
Trauma
If you were in a recent traumatic injury, such as a motor vehicle accident or a major fall, an x-ray should be used to rule out a fracture or dislocation. A proper evaluation can help determine if a fracture is likely and then an x-ray can help confirm a practitioner’s diagnosis.
-
Not Improving
If you have been receiving conservative care and you haven’t improved during a 4–6-week span, an x-ray can be useful to determine if you have a structural pathology (arthritic changes, stenosis, etc.) causing your symptoms.
“Most diagnostic images that were considered appropriate for the patient to get were those following failure of conservative care options therapy.
What are typical conservative care options?
- Chiropractic care
- Physical therapy
- Massage
- Pilates
- Yoga
- Low impact exercise” (1)
When can imaging be detrimental?
As mentioned above, x-rays are overly used in a variety of healthcare settings, especially in musculoskeletal and orthopedic fields. It should only be used to rule in or rule out a certain diagnosis that a clinician thinks is relevant based on their history and exam findings. The current literature shows that overuse of diagnostic imaging leads to more problems than it solves.
“It’s just a picture, why not just take one?”
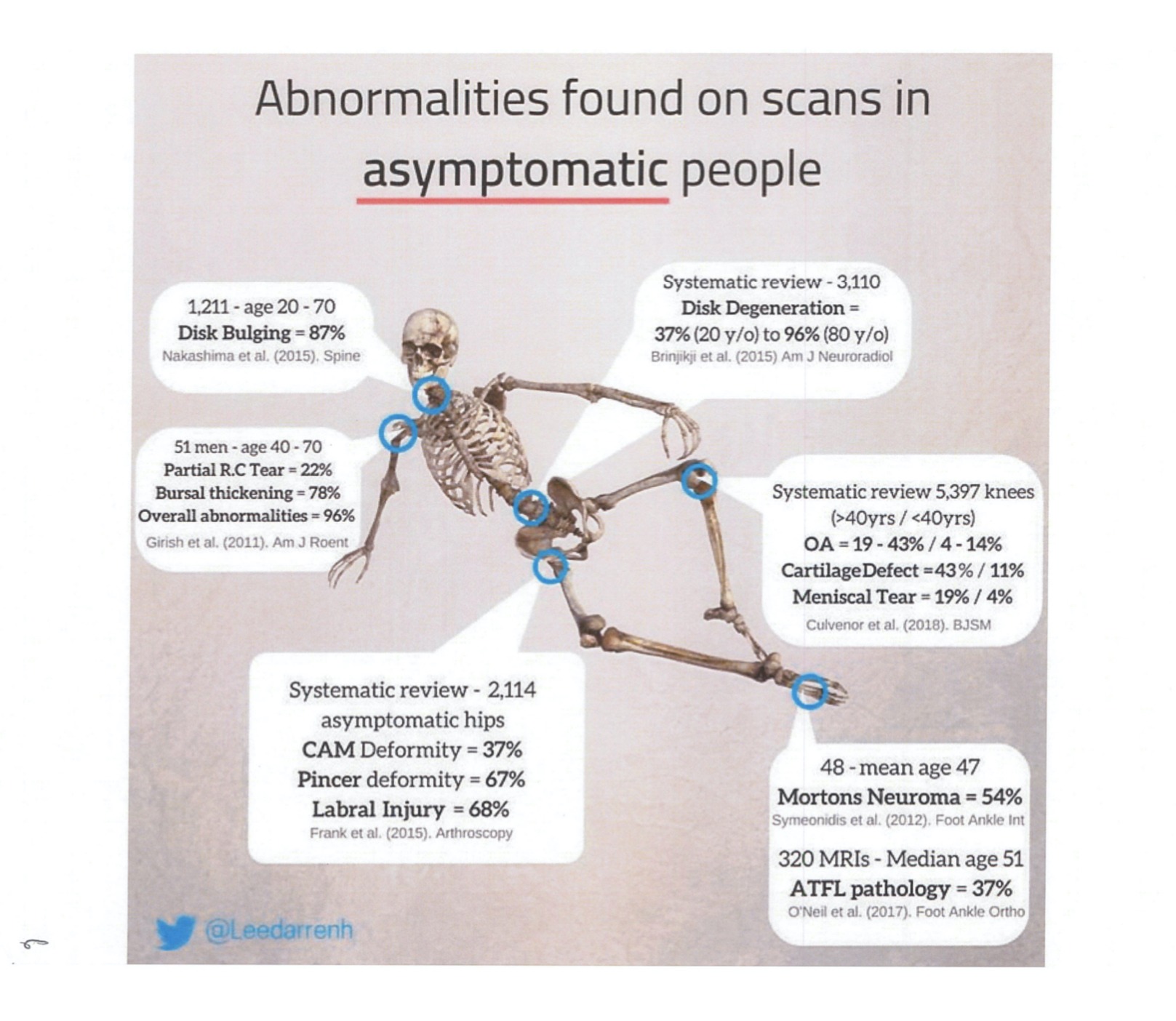
You might think it’s just an image, but that image can have a great impact on your care. Diagnostic imaging can lead to overdiagnosis, meaning you could have some structural differences that are normal to you, such as your spinal curvature or arthritic changes. Although it can show up on an image, it may not be causing your symptoms. The aforementioned examples are often used to explain why patients are having their symptoms. Did you know arthritis is a normal aging process, and that spinal curvatures are all unique to the individual?
“Overdiagnosis occurs when diagnostic imaging detects incidental findings that are common in the asymptomatic population (eg, intervertebral disc degeneration) and provides the patient with a diagnostic label that brings them no benefit or causes harm.” (2)
What harm could it bring? Well, unnecessary x-rays or MRI’s do NOT improve patient outcomes and lead to UNECESSARY surgeries. In other words, if you really want an x-ray or MRI, you likely really want to undergo surgery, whether it’s warranted or not. (3)
Don’t believe me? The research now shows “more than 50% of the patients indicated that they would undergo spine surgery based on abnormalities found on MRI, even WITHOUT symptoms.” (4)
Structure is a suspect but is rarely the culprit!
Diagnostic imaging should be used when structural pathologies or abnormalities are likely to be the cause. How do we know when they could be the culprit? If you failed conservative care (chiropractic or physical therapy) or were in a traumatic injury (accident).
Did you know a movement dysfunction is the most likely cause of musculoskeletal symptoms (pain and stiffness)?
A movement dysfunction can be characterized as a joint(s) that is not moving appropriately or as a joint(s) that is sensitized to certain movements or positions. Either dysfunction can lead to oversensitivity causing pain and muscle/joint stiffness.
That is why a proper movement assessment and physical exam are important during the first visit. An x-ray, or even an MRI, can’t tell me if you hurt during a certain movement or position. Evaluating you performing the movements or postures tells us way more information and helps guide your care more effectively.
For example, if you are only experiencing low back pain during a squat, that is a particular movement that is causing your symptoms. We wouldn’t need an x-ray to determine why it’s painful, we’d need to examine your squat to determine why it’s painful!
“Unnecessary diagnostic imaging for low back pain drives flow-on effects such as:
-
- Overuse of advanced imaging (MRI, CT, etc.)
- Opioid prescriptions
- Spinal injections (epidural and cortisone)
- Spinal surgery
Evidence from clinical guidelines suggests that most of these interventions have little to no benefit, and substantial risk for harms, in patients with non-specific low back pain.” (3)
How can we help?
Pain and stiffness can be difficult to treat on your own because you must first identify the source(s).
A clinician trained in Mechanical Diagnosis and Therapy (MDT) can clarify where the symptoms are coming from, getting to the root cause of your problem. An MDT practitioner can also determine if you’re experiencing a movement dysfucntion or a structural issue within 1-2 weeks and can determine if diagnostic imaging is the best thing for you.
Knowing the cause(s) of symptoms ensures the proper application of the best treatments and strategies to correct the problem as quickly as possible.
Hands-on active treatments with specific exercises have been proven to be the most effective for muscle, joint and back pain. In rare cases is surgery absolutely needed. Can you imagine how many surgeries have been performed where conservative treatments wheren’t utilized first?
When is surgery the better treatment option? When conservative treatments fail!
Pain is frustrating. At REACH, we take the guesswork out of healing. We use a holistic chiropractic approach, assessing the body as a whole rather than treating just the symptoms. So you can do more than relieve pain. We teach you how to become unstoppable.
References:
- Traeger AC, Reed BJ, O’Connor DA, Hoffmann TC, Machado GC, Bonner C, Maher CG, Buchbinder R. Clinician, patient and general public beliefs about diagnostic imaging for low back pain: protocol for a qualitative evidence synthesis. BMJ open. 2018 Feb 1;8(2):e019470.
- Sharma S, Traeger AC, Reed B, Hamilton M, O’Connor DA, Hoffmann TC, Bonner C, Buchbinder R, Maher CG. Clinician and patient beliefs about diagnostic imaging for low back pain: a systematic qualitative evidence synthesis. BMJ open. 2020 Aug 1;10(8):e037820.
- Nevedal AL, Lewis ET, Wu J, Jacobs J, Jarvik JG, Chou R, Barnett PG. Factors influencing primary care providers’ unneeded lumbar spine MRI orders for acute, uncomplicated low-back pain: a qualitative study. Journal of General Internal Medicine. 2019 Dec 12:1-8.
- Yates M, Oliveira CB, Galloway JB, Maher CG. Defining and measuring imaging appropriateness in low back pain studies: a scoping review. European Spine Journal. 2020 Mar;29(3):519-29.


